“We hear about gut health everywhere — but do we actually know what the gut is?”
Is it the stomach?
The intestines?
The bacteria?
Yes. And more.
Most of us grew up hearing about the stomach, the small intestine, or maybe the “digestive system” in biology class. But what we now know is that the gut is more than a food pipe — it’s a dynamic, intelligent system that influences nearly every aspect of health.
So let’s start with the basics: what exactly is the gut?
So, What Is “the Gut”?
When we say “gut,” we’re referring to the gastrointestinal (GI) tract — a muscular tube that runs from your mouth to your anus. It includes:
- Mouth
- Esophagus
- Stomach
- Small Intestine
- Large Intestine (Colon)
- Rectum and Anus
But the gut isn’t just a hollow tube.
It also includes:
- The Enteric Nervous System (ENS) — a vast web of over 500 million neurons embedded in the walls of the gut, often called the second brain[^1]
- The gut microbiota — trillions of microbes (mostly bacteria) living in the intestines
- Specialized gut cells that help regulate digestion, hormone release, and immune signaling
While these are part of the gut itself, the gut also works in close connection with:
- The immune system — About 70% of the body’s immune cells are located in the gut, primarily within gut-associated lymphoid tissue (GALT)[^2].
- The endocrine system —The gut acts like a mini endocrine system — producing ghrelin in the stomach[^3], a hormone that signals hunger, and GLP‑1 in the intestines, which helps regulate satiety, blood sugar, and digestion[^4].
- The central nervous system (CNS) - It communicates with the gut via the gut–brain axis, a bidirectional network that includes the vagus nerve — the main parasympathetic pathway between the two systems[^5].
These systems aren’t anatomically part of the gut, but they are deeply integrated with how the gut functions. Scientists often refer to them as the gut-immune, gut-brain, and gut-endocrine axes.
So, the gut is more than just a digestive tract.
It’s a neurochemical command center, a microbial metropolis, and a bridge between your internal and external world.
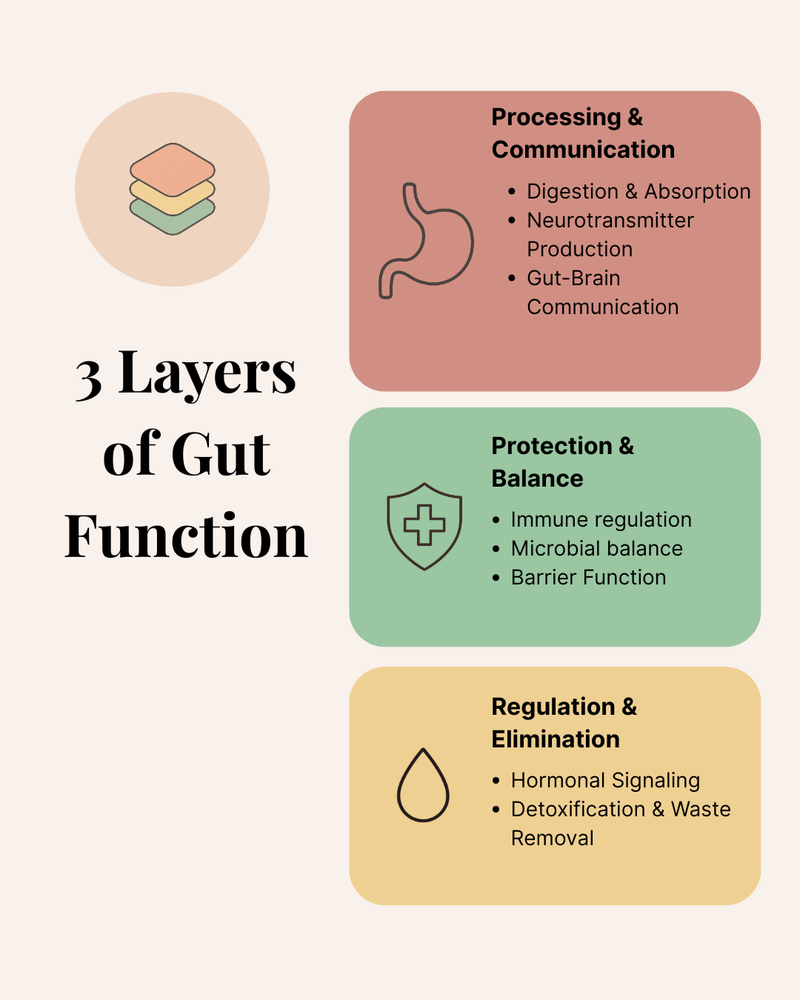
The Gut’s 3 Layers of Function
The gut is far more than a digestion pipe. It’s a multifunctional system — intelligent, adaptive, and constantly communicating with the rest of your body. To understand it fully, it helps to group its roles into three interconnected layers.
Layer 1: Processing & Communication
Digestion & Absorption
At its most fundamental level, your gut breaks down food into usable nutrients — amino acids, fatty acids, vitamins, minerals — and absorbs them into the bloodstream. These nutrients are what fuel your cells, repair tissues, and support every system in the body. Without proper digestion and absorption, even the best food can’t nourish you.
Neurotransmitter Production
Your gut is more than a digestion organ — it’s also a neurochemical powerhouse. The majority of your body’s serotonin (up to 95%) is synthesized in the intestinal tract by enterochromaffin cells, influencing mood, digestion, and immune response. Additionally, the gut serves as a hub for dopamine and GABA production: gut microbes and epithelial cells help regulate these neurotransmitters, which shape everything from motivation and focus to calm and rest within the gut–brain axis[^6][^7][^8].
Gut-Brain Communication
Through the vagus nerve, hormonal messengers, and immune signals, your gut is in constant dialogue with your brain[^9]. This two-way relationship — known as the gut-brain axis — explains why stress can disrupt digestion, and why gut imbalances can contribute to anxiety, depression, and brain fog.
Layer 2: Protection & Balance
Immune Regulation
Roughly 70% of the body’s immune cells are located in the gut-associated lymphoid tissue (GALT)[^10].Here, your body learns to distinguish friend from foe — tolerating helpful microbes and neutralizing pathogens. A well-regulated gut immune system prevents chronic inflammation and overreactions like food sensitivities.
Microbial Balance
The gut hosts trillions of microbes — the collective gut microbiota — that digest fiber, synthesize key vitamins, and help regulate immunity[^11]. A diverse, balanced microbiome supports health; an imbalanced one (dysbiosis) is linked to conditions like IBS, obesity, and autoimmune diseases.
Barrier Function (“Leaky Gut” Defense)
The inner lining of the gut is only one cell thick — yet it protects the body from pathogens, toxins, and undigested food particles. This barrier is supported by tight junction proteins, mucosal immunity, and beneficial microbes. When the gut barrier is compromised (a state commonly called “leaky gut”, it is a popular term for intestinal permeability and is still debated in some scientific circles.), it can allow harmful microbes, toxins, or undigested food particles to enter the bloodstream, potentially triggering widespread immune activation and inflammation[^12].
Layer 3: Regulation & Elimination
Hormonal Signaling
The gut acts like an endocrine organ, producing a wide array of hormones that regulate appetite, satiety, insulin sensitivity, and digestive flow—hormones like ghrelin, GLP‑1, and PYY work together to signal your brain about hunger and fullness[^13]. Gut hormone dysregulation is closely tied to metabolic disorders like obesity and type 2 diabetes.
Detoxification & Waste Removal
Your gut helps the body eliminate waste — not just leftover food, but also microbial byproducts, excess hormones, and bile-bound toxins. The colon, along with the liver–bile–gut axis, ensures efficient removal. If elimination is sluggish (e.g., constipation), toxic substances may be reabsorbed — burdening the liver and other systems[^14].
Why This Matters?
When you support your gut, you’re not just aiding digestion. You’re influencing your immune strength, emotional well-being, nutrient status, and long-term health risk. Understanding these core functions gives you more agency over your health — meal by meal, habit by habit.
We’ve touched on the trillions of microbes that live inside you — but they deserve a spotlight of their own. In the next article, we’ll explore the gut microbiome: what it is, what it does, and how to nourish it.
Share this article