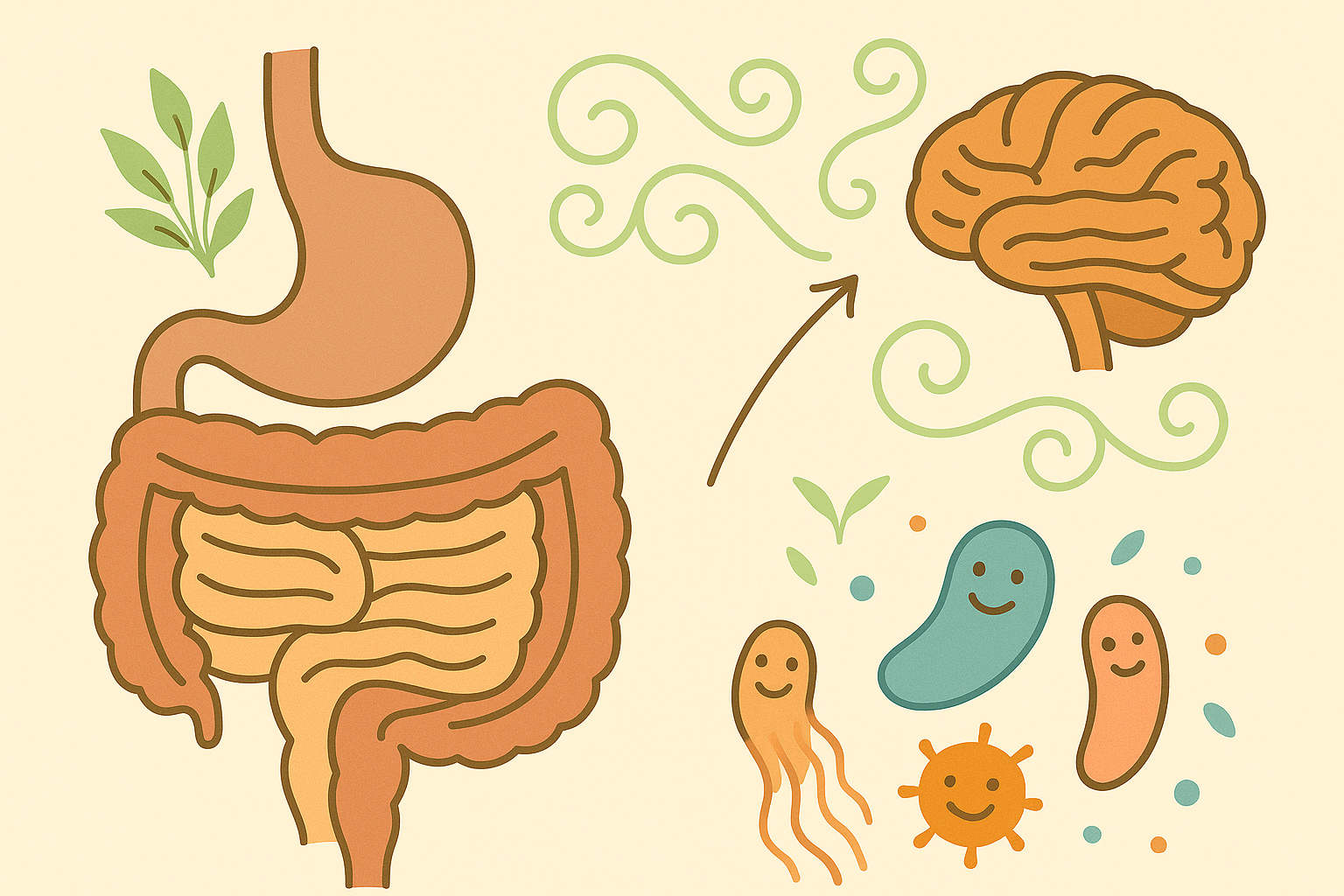
What if our health wasn’t just about us — but about the trillions of microbes living inside us? These invisible companions — collectively known as the gut microbiome — aren’t just along for the ride. They digest fiber, produce vitamins, regulate immunity, influence our mood, and help our bodies function in ways we’re only beginning to understand. So what exactly is this inner ecosystem? Let’s take a closer look.
What Is the Gut Microbiome?
Our gut microbiome is the collection of trillions of microorganisms that live in our digestive tract — mostly in the large intestine. It includes:
- Bacteria (the most studied)
- Fungi
- Viruses
- Archaea
- And even small parasites (in healthy balance)
Together, they outnumber our human cells and weigh about as much as our brain.
Why Does It Matter?
These microbes aren’t passive passengers. They’re biochemical workers — constantly digesting, fermenting, signaling, and producing compounds that influence our health.
Here’s just a glimpse of what they do:
- Digest fiber into short-chain fatty acids (SCFAs) like butyrate, which fuel colon cells and reduce inflammation
- Synthesize vitamins like B12, K2, and folate
- Modulate immune responses, teaching our body what to tolerate and what to attack
- Help maintain gut lining integrity, preventing leaky gut
- Influence metabolism and fat storage
- Produce neurotransmitters like GABA and serotonin
- A healthy microbiome is like a well-balanced community — diverse, stable, and functionally rich.
Is Everyone’s Microbiome the Same?
No — each person’s microbiome is as unique as a fingerprint.
It’s shaped by factors like:
- How we were born (vaginal birth vs. C-section)
- Whether we were breastfed
- Our early environment (urban vs. rural, pets, siblings)
- Our diet (fiber-rich vs. processed, fermented foods or not)
- Medication use (especially antibiotics, PPIs, steroids)
- Stress and sleep patterns
- Exposure to microbes in nature or through travel
This uniqueness helps explain why some of us can eat certain foods with no issue, while others experience bloating, sensitivities, or inflammation.
Is Our Microbiome Fixed or Flexible?
That’s the good news: it’s not fixed.
Our microbiome can change and adapt — sometimes within days — based on:
- What we eat
- How stressed we are
- How well we sleep
- Our exposure to different microbes (e.g., gardening, fermented foods, travel)
That means it’s possible to nurture our microbiome — or neglect it — through our daily habits.
Research shows that higher microbial diversity is linked to:
- Lower risk of metabolic disease[^1]
- Reduced inflammation [^2]
- Better weight regulation [^3]
- More resilient mood and cognition [^4]
- Stronger immunity[^5]
What Disrupts the Microbiome?
If our gut microbiome is an ecosystem, it thrives on balance and variety. But modern life can throw that balance off. Some of the most common microbiome stressors include:
- Highly processed, low-fiber diets
- Excess sugar and refined carbohydrates
- Chronic stress (which alters gut–brain signaling and gut motility)
- Frequent antibiotic use (which kills off both good and bad bacteria)
- Sleep disruption and circadian rhythm misalignment
- Environmental toxins and pollutants
- Sedentary lifestyle and lack of microbial exposure
Over time, these can lead to dysbiosis — a disrupted microbial balance — which is linked to symptoms like bloating, fatigue, inflammation, skin issues, and mood imbalances.
The good news? Just as our microbiome can be harmed by our habits, it can also be healed by them. You don’t need perfect routines — just consistent, nourishing ones.
What Makes a Microbiome Healthy?
A healthy gut microbiome isn’t just about having more microbes — it’s about having the right mix, with enough diversity, stability, and functional activity to support our body’s needs.
Some key features include:
- A high count of fiber-fermenting bacteria (like Bifidobacteria)
These species break down plant fibers into short-chain fatty acids (like butyrate), which fuel gut cells, reduce inflammation, and support immune health.
- Presence of butyrate-producing species (like Faecalibacterium prausnitzii)
Butyrate is one of the most important postbiotic compounds for gut health. It strengthens the gut lining, lowers inflammation, and even supports brain health via the gut–brain axis.
- Low abundance of inflammatory or opportunistic microbes (like Clostridium difficile)
These microbes are naturally present in small numbers, but if they overgrow — often due to antibiotics, stress, or poor diet — they can disrupt the ecosystem and trigger symptoms or disease.
- Richness across phyla — not dominated by just a few species
Microbial diversity is like biodiversity in a rainforest: the more variety, the more resilient and adaptive the system. A rich microbiome can perform a wider range of functions and adapt better to change.
You won’t see any of this on a nutrition label — but our daily choices are constantly shaping it. What we eat, how we live, how we rest — it all sends a message to the microbial world inside us.
Final Thought
Our microbiome is always changing — and it’s always listening. It listens to what we eat. When we sleep. How we feel. Whether we rest or rush. The choices we make each day — in the kitchen, at the table, in our thoughts — are shaping an inner ecosystem that affects nearly everything else. We don’t need perfect habits. Just consistent ones. So, what kind of community are we feeding today?
Coming Up Next
In this article, we’ve only scratched the surface of the microbiome’s power — and how much it shapes our health.
From how it digests fiber… to how it regulates inflammation… to the way it communicates with our brain, immune system, and metabolism — this inner ecosystem is constantly working behind the scenes.
But what happens when things go off balance?
In upcoming articles, we’ll explore:
- Dysbiosis — what it is, how it happens, and what it feels like
- The gut–brain axis — and why the microbiome is sometimes called our second brain
- Short-chain fatty acids (SCFAs) — the postbiotic heroes behind gut healing
- Fiber, fermented foods, and microbial diversity — how our diet shapes our microbial world
- And most importantly: how to nourish our gut — meal by meal, habit by habit
The gut is a living system. Let’s learn how to care for it — together.
Share this article